Everything is changing in medicine, more now than ever, and change is hard. New technology is not always welcomed by people who have to use it, new research comes out so fast it is impossible to keep up, methods of payment are tedious to say the least in some countries, and now patients are changing too. These new patients want to be involved in their own care and are trying to equip themselves to do it.
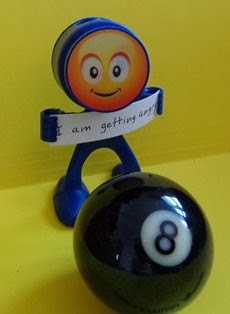
It's hard for all of us to do this. To help us I like this unofficial slogan of the Marines "Adapt. Improvise. Overcome." We can use it for ePatient Boot Camp.
The "E" s I propose for health care professionals are these:
Some examples of situations where the above qualities were not evident follow below. These situations are hopefully few and far between but always hard to forget.
Change can be good
It's hard for all of us to do this. To help us I like this unofficial slogan of the Marines "Adapt. Improvise. Overcome." We can use it for ePatient Boot Camp.
ePatient
The "E" s I propose for health care professionals are these:
Encourage, Empathize, Educate, Engage
She has found a great medical team which works with her and often her doctors have Fellows training with them. If she is feeling good enough the doctor will direct the Fellow to examine her as a learning experience for him or her.
Recently a Fellow, after examining her and looking at the chart, described her condition as stable. Her response: "Don't you be saying that about me," and she proceeded to lecture him about the profound changes that her illness has had on her life and how much she has had to adapt, even to the extent of moving from a two-story house to a bungalow.
She said "It's hard to have your life upended. I've had six esophageal spasms since I was here last not to even mention other symptoms. This is not stable" Her doctor came in at the tail end and said, "Aah, I see he described you as stable."
Here's a snapshot of a moment with a specialist who I see. He was teaching a group of students and talking about
the effects of wrist fusion. He said to the students "Don't worry about personal care.
They'll figure it out."
I told my "unstable" friend the story and she said "That's obscene" How little effort it would take to tell these future surgeons this instead: "Some patients may worry about personal care. You could suggest they talk to an occupational therapist if it continues to be a problem."
Her
friend Terri who lives in a small town went to see her
rheumatologist. He was sitting in a very relaxed way at his desk, with
his hands behind his head. She offered him some pamphlets about
Sjogren's Syndrome. He stood up, said "Wait a minute" and walked over to
his diploma on the wall. He tapped it and then said "Who's the doctor here?"I told my "unstable" friend the story and she said "That's obscene" How little effort it would take to tell these future surgeons this instead: "Some patients may worry about personal care. You could suggest they talk to an occupational therapist if it continues to be a problem."
My favourite doctor says the hardest thing to teach is empathy. Perhaps more patient involvement in medical education would be helpful. Maybe learning first hand through narrative medicine about the Burden of Treatment (by Dr Victor Montori) for patients would help some professionals to take this step.
Burden of Treatment
Article: Clinical Empathy as Emotional Labor in the Physician-Patient Relationship