That plan has worked out well. I can stay abreast of what's new and it's easy to share on Twitter. You might wonder how I choose among all the new papers. It's easy - I pick what interests me. Here are some reasons for avoiding certain topics.
First I don't post animal tests because I want to find knowledge that is closer to being applicable to people like me.
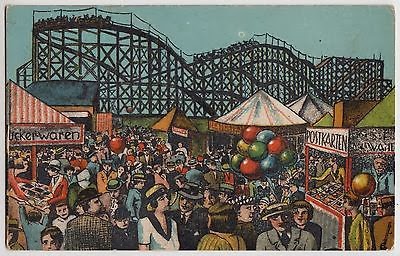
We could test on this rat
Second I need to have at least some understanding of the subject matter. That's why I did not post this one:
Rho-GTPase signaling in leukocyte extravasation: An endothelial point of view.
Extravasation?
Third, case studies don't seem broadly relevant to me as a patient.
Finally I want to learn something from the links I find, even if it's only a small insight or fact.
Here's an example of a study I plan to Tweet:
A proof-of-concept study of ANSWER, a web-based methotrexate decision aid for patients with rheumatoid arthritis.
"For patients with rheumatoid arthritis (RA) who are considering
methotrexate, we have developed a web-based patient decision aid called
the ANSWER (Animated, Self-serve, Web-based Research Tool)"
When I first heard of decision aids I was really excited by the concept until I found out that we were talking about pamphlets. There's been a lot of progress since that day years ago and now you can find interactive fact-based online tools that are truly geared to the needs of an individual. The ANSWER paper tested a method of helping patients choose whether or not to take the usual first step in the treatment of RA: using methotrexate.
When I looked for more information (partly because I liked the poster picture) I found another paper by Dr Li that provided more background about the usability testing of this tool. That's the beauty of looking on the internet - you usually find even more than you expect.
That's why the above link is the perfect choice. This research is done by Arthritis Research Canada in BC so it's Canadian and very applicable to people I often talk to online. Of course the decision whether or not to take methotrexate is one I made long ago, but it applies directly to people with a new diagnosis of RA, and there are many of them online.
My theory is that it's harder to find answers when you don't know the questions. That's one of my reasons I like to share useful tools and answers I find on the internet.
Also when I start my searches with links to papers published in a journal that is included on PubMed it makes me feel more comfortable with the likelihood that the facts are accurate.
And here's the link to where you can actually try this web-based decision aid yourself :
Answer Tool at ARC Canada
And here's the link to where you can actually try this web-based decision aid yourself :
Answer Tool at ARC Canada
Crossroads picture from ARC, others my own